NCPV releases first batch of X-ray inactivated SARS-CoV-2 (Strain B.1.1.7/N501Y/V1 Kent/Alpha)
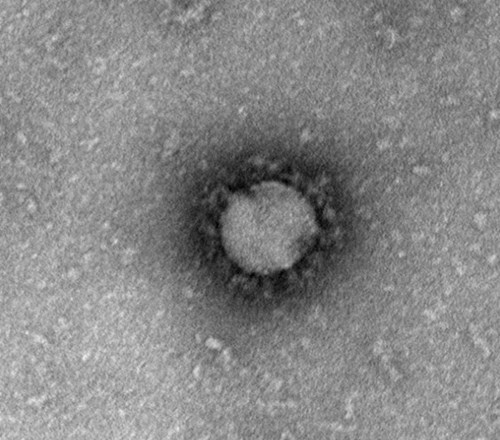
SARS-CoV-2 is a hazard group 3 pathogen, mandating all work with infectious materials be performed in specialist Containment Level 3 laboratories. Inactivating the virus substantially decreases the barrier for laboratories who wish to study the virus and increases the breadth of analyses possible.
Standard methods used to inactivate SARS-CoV-2 include heat, and chemical agents such detergents, Trizol or chemical crosslinking of surface proteins with formaldehyde. Unfortunately, these methods denature or significantly modify proteins such that many native antigenic structures are lost. This is especially problematic if inactivated pathogens are being used for clinical diagnosis and reference virology.
X-ray irradiation offers a superior quality of non-infectious native reagents since antigenic structure is maintained. Importantly no residual toxic chemicals are present in the preparation to interfere with any subsequent assays, opening a multitude of downstream detection and functional evaluations, since key biochemical and immunological properties are preserved. An additional advantage is that x-ray inactivated virus preparations retain enough intact nucleic acid to enable full genomic sequence reconstruction, supporting their use as positive control reagents in nucleic acid assay tests.
X-ray inactivation of SARS-CoV-2 has been determined by sterility assays in validated serial passage experiments in tissue culture. In addition to cytopathic effect in vitro, viral RNA and mRNA have been used as sensitive markers of viral replication and provide evidence that this approach produces inactivated SARS-CoV-2 for use outside of containment.
The production of non-infectious material containing whole-virus characteristics is a distinct advantage as it supports more complex experimental strategies than can be achieved with chemically modified or heat-denatured inactivated viral material. UKHSA have also conducted additional studies examining the parameters that influence direct or indirect mechanisms of viral inactivation by x-rays, such as sample types and suspension matrices, physiological temperature states, particle size and infectious titer. Our work has determined that x-ray irradiation can rapidly advance and strengthen conventional public health laboratory activities for pathogen inactivation1.
Pathogen inactivation by exposing it to a specific dose of ionising radiation sufficient to render the pathogen biologically non-infectious, but not enough to destroy its structural integrity (such that research on it would still be insightful and accurate) has been attempted previously using 60Co or Cs137 gamma rays. However, such sources of ionising radiation are themselves associated with drawbacks, such as security concerns, decay, and waste management; indeed, the UK Government, along with other countries, is currently investigating ways of replacing the radionuclide irradiators used in radiobiology for precisely these reasons. Moreover, although filters may potentially be added to change the characteristics of radiation, emission from a radionuclide source is essentially of fixed quality. Importantly x-rays do not have the same disadvantages and can be fine-tuned to match precise dosimetry requirements.
The success of the x-ray approach has relied upon detailed microbiology, accurate measurements of inactivation and the precision of delivery and quantification of x-ray doses2. It has been developed through a highly effective collaboration between HSA institutes at Porton and Chiltern.
Additional pathogens inactivated with x-irradiation will be made available through NCPV soon.
References:
1. Afrough B, Eakins J, Durley-White S, Dowall S, Findlay-Wilson S, Graham V, Lewandowski K, Carter DP, Hewson R. X-ray inactivation of RNA viruses without loss of biological characteristics. Sci Rep. 2020 Dec 8;10(1):21431. doi: 10.1038/s41598-020-77972-5. PMID: 33293534; PMCID: PMC7722841.
2. Eakins JS, Afrough B, Hewson R. Monte Carlo modelling of an x-ray chamber for providing inactivation exposures to viruses. J Radiol Prot. 2021 Nov 11;41(4). doi: 10.1088/1361-6498/ac2f85. PMID: 34644683
UKHSA, Virology & Pathogenesis group
